Understanding Diabetic Foot Ulcers: Causes, Management, and Prevention
This blog is dedicated to providing a comprehensive overview of diabetic foot ulcers. We will explore the underlying causes, pathophysiology, and different types of diabetic foot ulcers. We will also discuss effective management strategies, prevention measures, and the potential need for amputation in severe cases. Whether you are a healthcare professional or someone living with diabetes, this blog will offer valuable insights into this common complication.
Introduction: Diabetic foot ulcers are a common and serious complication of diabetes. They can lead to debilitating pain, infections, and even amputations. According to the World Health Organization, an estimated 15% of people with diabetes will develop foot ulcers during their lifetime. This blog aims to provide a thorough understanding of diabetic foot ulcers, including their causes, pathophysiology, and management.
Epidemiology: Diabetic foot ulcers are a major public health concern worldwide. In the United States alone, foot ulcers affect up to 25% of people with diabetes. They are more common in older adults, those with long-standing diabetes, and those with poor blood sugar control. Other risk factors include neuropathy, peripheral arterial disease, foot deformities, and smoking.
Pathophysiology: The development of diabetic foot ulcers is multifactorial. Chronic hyperglycemia can lead to neuropathy, which can cause loss of sensation and reduced blood flow to the feet. This can make it difficult for patients to notice cuts, blisters, or other injuries. Additionally, high blood sugar levels can impair wound healing and make infections more likely.
- In the development of neuropathy, the hyperglycemic state leads to an increase in action of the enzymes aldose reductase and sorbitol dehydrogenase. This results in the conversion of intracellular glucose to sorbitol and fructose. The accumulation of these sugar products results in a decrease in the synthesis of nerve cell myoinositol, required for normal neuron conduction. Additionally, the chemical conversion of glucose results in a depletion of nicotinamide adenine dinucleotide phosphate stores, which are necessary for the detoxification of reactive oxygen species and for the synthesis of the vasodilator nitric oxide. There is a resultant increase in oxidative stress on the nerve cell and an increase in vasoconstriction ion leading to ischemia, which will promote nerve cell injury and death(Warren Clayton et al,2009)
- Neuropathy in diabetic patients is manifested in the motor, autonomic, and sensory components of the nervous system
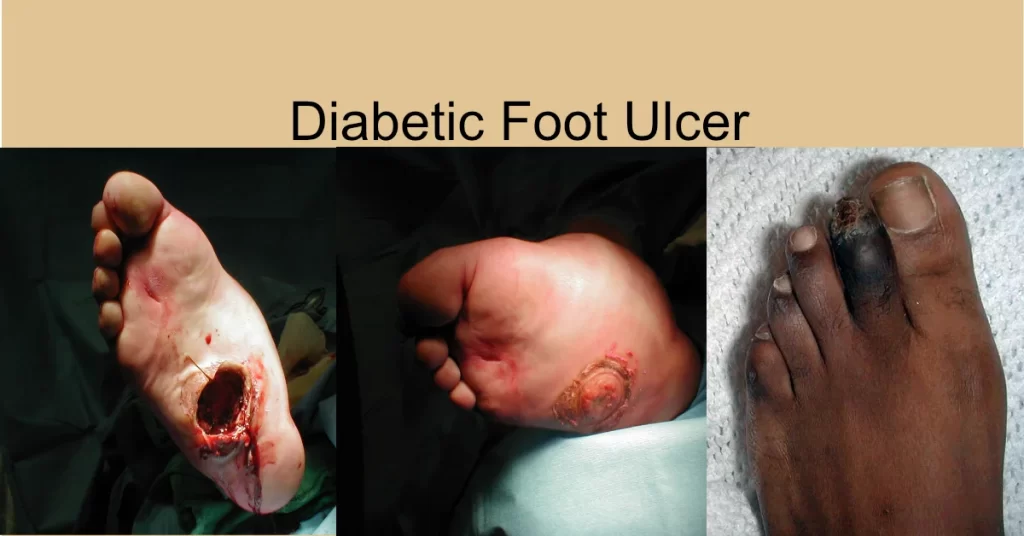
Types of diabetic foot ulcers: There are several types of diabetic foot ulcers, each with its own unique characteristics. These include neuropathic ulcers, ischemic ulcers, and neuroischemic ulcers.
- Neuropathic ulcers are the most common type, more than 60% of DFU results from neuropathy and are usually located on the sole of the foot.
- Ischemic ulcers typically occur on the toes or heels and are caused by reduced blood flow.
- Neuro-ischemic ulcers are a combination of the two.
Ulcers classification: Diabetic foot ulcers are classified based on their depth and severity. The Wagner classification system is the most commonly used and ranges from grade 0 (pre-ulcerative lesions) to grade 5 (gangrene or extensive tissue loss). Other classification systems include the University of Texas system and the PEDIS classification.
Wagner classification
- Superficial diabetic ulcer
- Ulcer extension involving ligament, tendon, joint capsule, or fascia with no abscess or osteomyelitis
- Deep ulcer with abscess or osteomyelitis
- Gangrene to portion of forefoot
- Extensive gangrene of foot
Management according to classification: Effective management of diabetic foot ulcers requires a multidisciplinary approach. Treatment may include offloading, wound debridement, antibiotics, and surgery. The choice of treatment depends on the severity of the ulcer and underlying conditions such as neuropathy or peripheral arterial disease.
Prevention from primary to tertiary: Preventing diabetic foot ulcers is essential for reducing the risk of complications. This includes regular foot exams at least annually, proper footwear, blood sugar control, and smoking cessation. Patients with neuropathy or peripheral arterial disease may require additional preventive measures, such as foot orthotics or vascular interventions.
Note: Diabetic foot risk classification system, designed for to make basic recommendations regarding the need for specialist referral and the frequency of follow-up by primary providers and specialists.It has 4 categories (0-3) based on loss of protective sensation (LOPS), foot deformity, peripheral arterial disease (PAD).
Charcot foot: Charcot foot is a rare but serious complication of diabetes that can lead to deformity and disability. It is characterized by bone and joint destruction caused by repeated trauma and poor healing. There are two theories for the development of Charcot foot:
- Neuro-traumatic theory; where Decreased sensation + repetitive trauma = joint and bone collapse
- Neurovascular theory; Increased blood flow → increased osteoclast activity → osteopenia → Bony collapse
OR Glycolization of ligaments → brittle and fail → Joint collapse.
Classifications: Charcot foot is classified based on the location and extent of bone and joint destruction. The most commonly used classification system is the Eichenholtz system, which ranges from stage 0 (pre-destructive) to stage 3 (reconstruction).
- Inflammatory
- Fragmentation
- Coalescence
- Consolidation
Indications for amputation: In severe cases of diabetic foot ulcers, amputation may be necessary to prevent further complications. Indications for amputation include extensive tissue loss, severe infection, and uncontrolled pain. The decision to amputate is made on a case-by-case basis.





Responses