Understanding Ascites: Anatomy, Causes, Diagnosis, and Management
In this blog, we will discuss a medical condition known as ascites. We will dive into the anatomy of the peritoneal cavity, the production of peritoneal fluid, and the meaning of ascites. We will also explore the various causes, pathophysiology, classification, diagnosis, investigations, ascites fluid analysis, management, and complications of ascites.
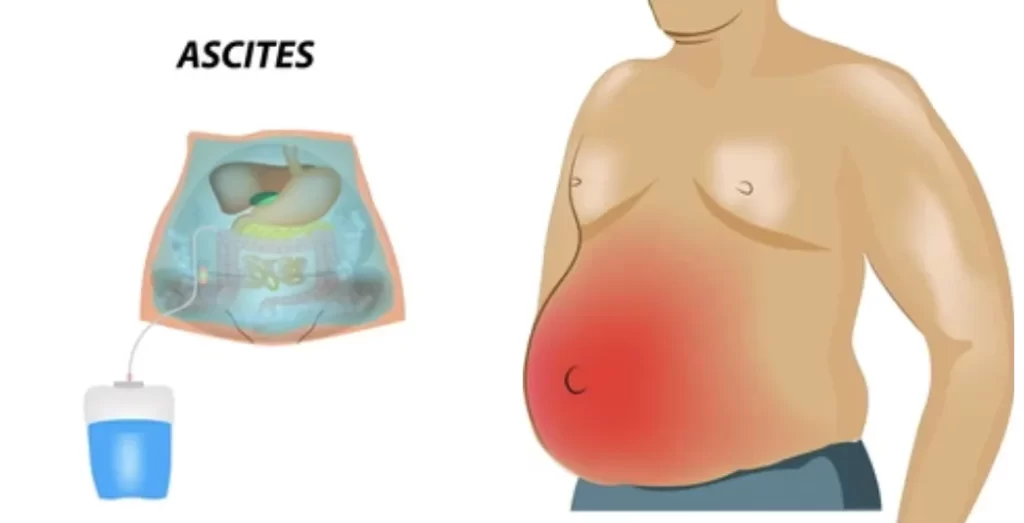
Introduction: Ascites is a medical condition that refers to an abnormal accumulation of fluid in the peritoneal cavity, which is the space between the abdominal organs and the abdominal wall. This buildup of fluid can result in abdominal swelling, discomfort, and other complications. Ascites is often associated with liver disease, but it can also be caused by other medical conditions such as heart failure, kidney disease, and cancer. In this blog, we will explore the various aspects of ascites, including its anatomy, causes, diagnosis, and management.
Anatomy of Peritoneal Cavity and Peritoneal Fluid Production:
The peritoneal cavity is a a thin, fluid-filled space that surrounds the abdominal organs, such as the liver, stomach, and intestines. It is lined by a thin layer of tissue called the peritoneum. The peritoneum produces a small amount of fluid that helps to lubricate the organs and allows them to move smoothly. This peritoneal fluid is constantly being produced and reabsorbed by the body. The fluid also helps in the removal of waste products from the peritoneal cavity. However, in certain medical conditions, the balance between production and reabsorption is disrupted, leading to an accumulation of fluid in the peritoneal cavity.
Definition: Ascites is a medical condition that refers to the accumulation of excess fluid in the peritoneal cavity. It is often a sign of an underlying medical condition, such as liver disease or heart failure. Ascites can cause abdominal swelling, discomfort, and difficulty in breathing.
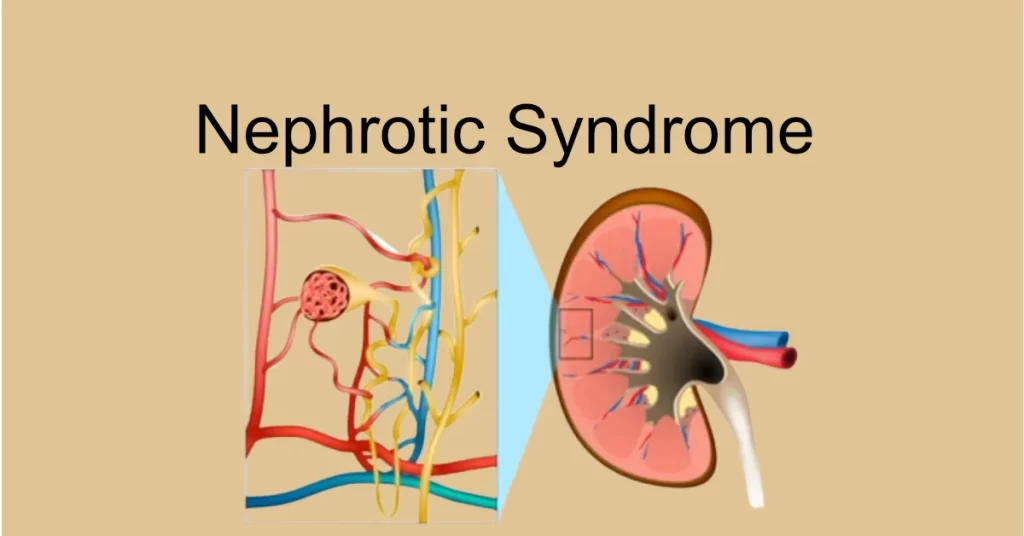
Causes: Ascites can be caused by various medical conditions, such as liver disease, heart failure, kidney disease, and cancer. In liver disease, such as cirrhosis, the liver is damaged and cannot function properly, leading to an accumulation of fluid in the peritoneal cavity. Similarly, in heart failure, the heart cannot pump blood efficiently, leading to an accumulation of fluid in the body, including the peritoneal cavity.
Other causes of ascites include heart failure, cancer, kidney disease, and infections such as tuberculosis or peritonitis. The condition can also develop as a result of certain medications or as a complication of surgery.
Pathophysiology: The pathophysiology of ascites involves the disruption of the balance between the production and reabsorption of peritoneal fluid. This disruption can be due to various medical conditions that affect the liver, heart, kidneys, or other organs.
Classification: Ascites can be classified based on the severity and underlying medical condition. The severity of ascites is often graded on a scale from 1 to 3, with grade 3 being the most severe. The most commonly used classification system is the one developed by the International Ascites Club. This system divides ascites into three grades, based on the amount of fluid present in the peritoneal cavity and the severity of symptoms. The underlying medical condition can also be used to classify ascites. For example, ascites associated with liver disease is called cirrhotic ascites, while ascites associated with cancer is called malignant ascites.
Ascites three grades:
- Grade 1: mild, only visible on ultrasound and CT – abdomen
- Grade 2: detectable with flank bulging and shifting dullness
- Grade 3: directly visible, confirmed with the fluid/wave thrill
Diagnosis: The diagnosis of ascites involves a physical examination, medical history, and various diagnostic tests. The physical examination may reveal abdominal swelling and fluid wave testing. Medical history can help identify underlying medical conditions that may be causing ascites. Diagnostic tests may include imaging studies such as ultrasound or CT scan, blood tests, and paracentesis.Investigations: In addition to the diagnostic tests mentioned above, other investigations may be required to determine the underlying cause of ascites. These investigations may include liver function tests, viral hepatitis testing, and endoscopy
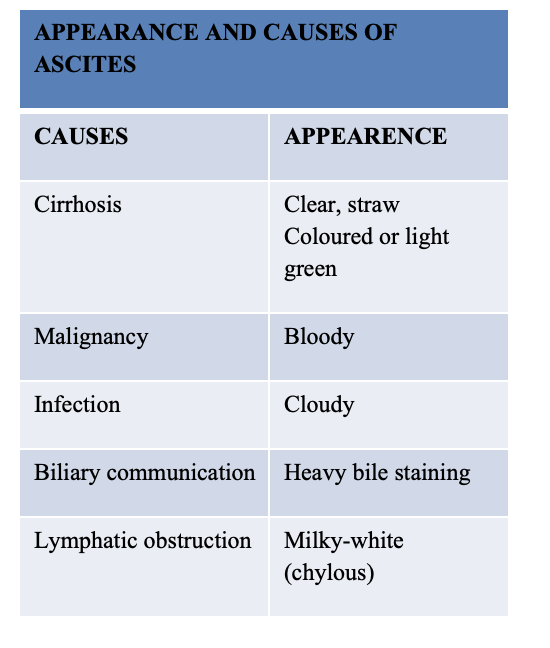
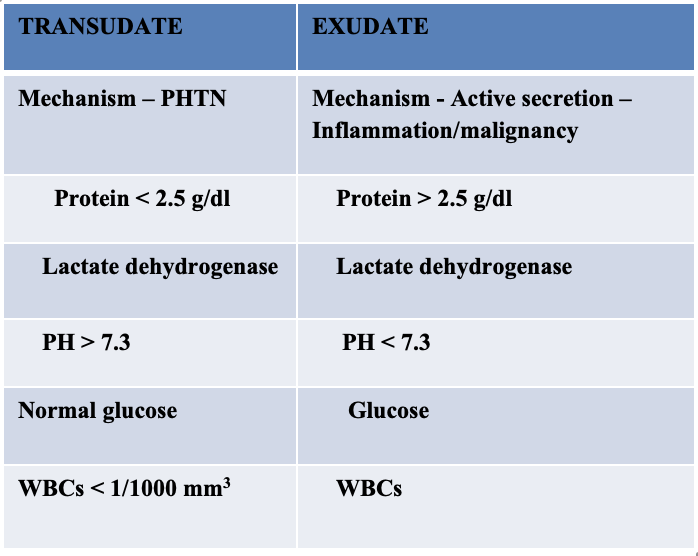
Ascites Fluid Analysis: Fluid analysis is an essential step in the diagnosis and management of ascites. The fluid is collected through a paracentesis procedure and analyzed for various parameters, including the total protein, albumin, and cell count. The results of the fluid analysis can help determine the underlying cause of the ascites and guide the management plan.
Serum-Ascites Albumin Gradient (SAAG): Best single test for classifying ascites into PHTN and non PHTN causes
Calculated by: Serum albumin – Ascites albumin= SAAG
- SAAG >1.1 g/dL= PHTN causes
- SAAG < 1.1 g/dL= Non-PHTN causes
Management: The management of ascites depends on the underlying cause and the severity of the condition. The primary goal of treatment is to reduce the amount of fluid in the peritoneal cavity and manage any underlying conditions. Treatment options mainly in (high SAAG “Transudate” ascetic fluid)may include diuretics, which help to remove excess fluid from the body, and paracentesis, which involves draining the fluid from the abdomen using a needle.
In more severe cases of ascites, surgery may be necessary to remove the excess fluid and repair any underlying damage. Other management options may include dietary changes, such as reducing sail intake. In severe cases, a shunt may be surgically implanted to redirect the excess fluid to another part of the body. In a minority of patients with advanced cirrhosis that have recurrent ascites, shunts may be used. Typical shunts used are;
- Portacaval shunt,
- Peritoneovenous shunt,
- Transjugular intrahepatic portosystemic shunt(TIPS).
Note: Low SAAG “exudate” Exudative ascites generally does not respond to manipulation of the salt balance or diuretic therapy.Repeated paracentesis and treatment of the underlying cause is the mainstay of treatment.
Complications of ascites can be serious and can include infection, spontaneous bacterial peritonitis, and hepatic encephalopathy. It’s important for patients with ascites to work closely with their doctors to manage the condition and prevent complications.
In summary, ascites is a medical condition that involves the accumulation of fluid in the peritoneal cavity. It can be caused by a number of different underlying medical conditions and can lead to a range of symptoms and complications. Early diagnosis and treatment are key to managing ascites and preventing complications.



Responses