Restorative dentistry as a risk factor for gingivo-periodontal diseases.
RISK FACTORS IN THE ETIOLOGY OF GINGIVOPERIODONTAL DISEASES.
A risk factor is one whose presence implies that there is an increase in the possibility of a certain disease occurring, in this case, gingiva-periodontal disease.
It acts as a predisposing or modifying factor that can accelerate the periodontal destructive process, which is always initiated by microbial factors.
Risk factors can be primary and secondary.
The primary risk factor is bacterial plaque or biofilm, i.e., the microbiota associated with gingiva periodontal disease.
Secondary risk factors include general and local risk factors. These are age, race, socioeconomic status, systemic conditions such as hormone levels, pregnancy, oral contraceptives, stress, smoking, diabetes, osteoporosis, HIV, leukemia, neutropenia, hypophosphatasia, genetic disorders with clinical translation such as Down syndrome, Papillon-Lefevre syndrome, or without clinical translation, such as diseases of the immune system.
Incorrect restorative dentistry, as well as inadequate oral hygiene, the presence of calculus, dental anatomy, dental malpositions, etc., are environmental factors that act as local risk factors.
The way in which periodontal disease progresses and the forms it assumes depend on the characteristics of the host.
Systemic factors can modify all forms of periodontitis, mainly through their effects on immunity and the inflammatory response.
Bacteria are necessary but not sufficient to cause periodontal disease; a susceptible host, a given time period, and a predisposing environment are required.
A periodontally healthy individual may have a potentially pathogenic bacterium, but if the environment and host response become risk factors, the bacterium could cause disease.
In individuals susceptible to developing periodontitis, bacterial plaque extends into the sulcus and forms subgingival plaque, which adheres to the tooth surface forming the biofilm.
Several environmental factors are capable of causing periodontal disease.
First of all, poor oral hygiene should be considered, which contributes to facilitating the deposition of plaque and calculus, thus increasing the total number of bacteria.
Dental restorations (margin adaptation, restoration contours, proximal relationship, and surface smoothness), orthodontics, and periodontal health are inseparably interrelated; they exert a critical biological impact on periodontal tissues.
Local environmental factors, therefore, have an important influence on maintaining periodontal health, which is necessary for the proper functioning of all restorations and their functional stimulation; it is essential for the preservation of the periodontium.
There is a periodontal dimension to every restoration, whether it partially or completely rebuilds a tooth.
In the final analysis, the periodontium is the testing ground for all restorative procedures.
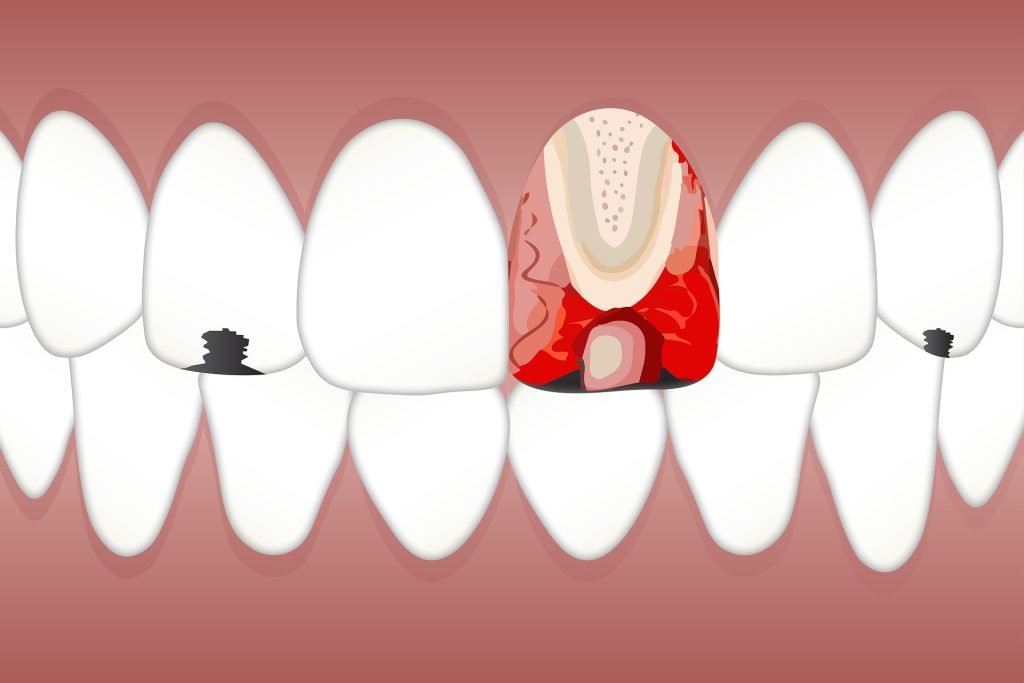
From what has been said so far, it is clear that improper restorative dentistry is a risk factor to be considered in the etiology of periodontal disease. Likewise, periodontal disease emerges as a relevant cause of the failure of restorative dentistry (Figs. 1A and B, 2A, B, C, and D). Failure is due more to biological causes than to mechanical reasons.
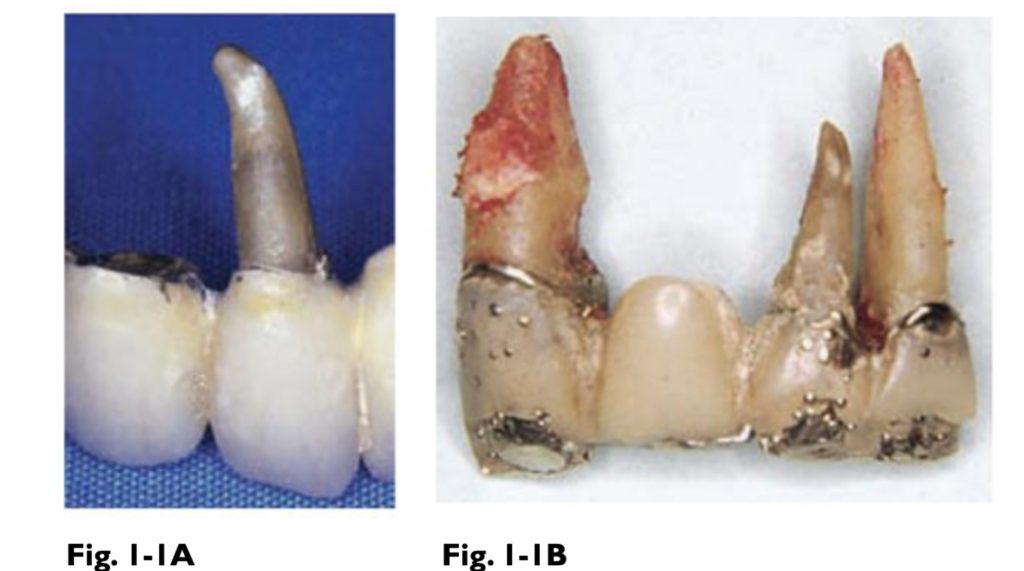
A. The failure of restorative dentistry is often due to periodontal-type lesions; therefore, we must keep certain requirements in order not to become a risk factor in the progression of periodontal disease. B. Although it is true that the bridge has failures due to wear of the esthetic material, its function was maintained until the loss of periodontal support.
In both cases, there is a total lack of periodontal ligament on the root surfaces of the abutment teeth.
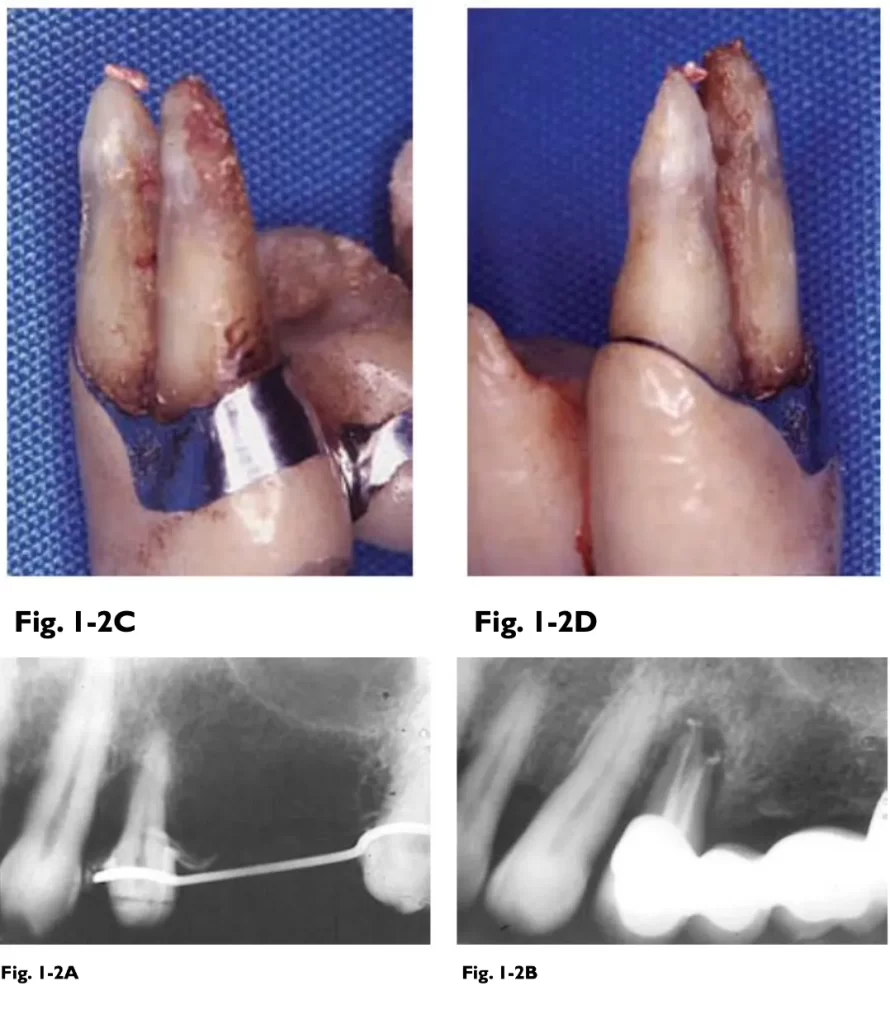
A. Periodontal treatment apparently succeeded in keeping the premolar and using it as an abutment tooth. B. Preventively, endodontic treatment was performed to avoid necrosis due to grinding or pulp involvement due to infection through the dentin ducts exposed to the pocket lumen. C and D. Bridge failure was due to periodontal reasons. As can be seen, some root surfaces were smoothed properly, while others showed coarse root debris. The failure of the bridge was due to periodontal reasons.
of calculus, especially in the vicinity of the furcation.. The teeth presented anatomical difficulties for scaling and root planing in order to achieve the final objective, i.e. disinfection of all root surfaces.
NORMAL GUM. THE STARTING POINT
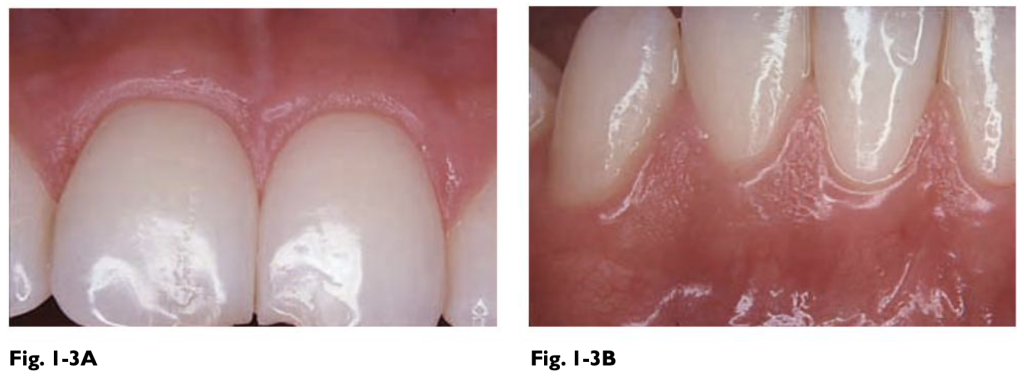
In normal gingiva, the papilla fills the proximal space and the margin ends in a bevel or knife-edge shape. The images show a healthy gingiva on a healthy tooth, with a dull surface appearance, the characteristic graining of the inserted gingiva, and the smooth appearance in the marginal gingiva. This is the way to start

These images of inflamed gingiva demonstrate the great difference from normal gingiva. The chronic inflammation transforms it into a red, smooth, soft, and shiny gingiva, the papillae appear enlarged and the graining of the inserted gingiva disappears.
Before any restorative procedure. The inserted gingiva is firm and resilient and is solidly attached to the periosteum of the alveolar bone. Its width varies according to the different areas of the mouth and its dimensions may change during the course of life. The presence of an adequate band of attached gingiva acts as an effective barrier to chewing trauma. The fundamental basis of this work is to give the necessary guidelines to maintain healthy gingiva in terms of its pale pink color, its finishing shape, regular concave arch, beveled shape, and firm, and resilient consistency.
It is unlikely that the patient will come to the office with healthy gingival margins when crowns are desired in the anterosuperior section.
The diagnosis will vary from gingivitis to periodontitis, being of utmost importance that a correct diagnosis is made and the corresponding therapy is initiated. Very often with mild gingivitis, the teeth are prepared, provisional restorations are made and definitive impressions are taken at the same appointment.
This type of procedure leads to failure, the inflammation complicates what should be simple, the impression-taking and the separation of the gingival margin.
The patient, by complying with the demands of hygiene, manages to eliminate plaque and if it continues with the economically expensive definitive restoration, the deflation of the tissues causes one of the most feared esthetic alterations, the retraction of the gingival margin. This can occur during the temporary veneering stage or after the cementation of the definitive restoration.
In both cases, it exposes the patient to fatal esthetic failure.
Therefore, in order to avoid periodontal failure, the following should be taken into account:
- Periodontal inflammation and periodontal lesions diminish the ability of the abutment teeth to respond to the functional demands of the prosthesis.
- Restorations built on healthy periodontium provide beneficial influences; on the other hand, they are destructive when placed on teeth affected by periodontal disease or generate it, shortening the life of teeth and prostheses.
- The periodontal disease is often disrupted in the tooth position, and the resolution of periodontal disease and the regeneration of periodontal tissues after treatment sometimes cause the teeth to return to their original place.
- Many teeth affected by periodontal disease have become excellent abutments after treatment.
- Partial dentures built on models made with the gingival and mucosal disease of the non-firm ridge cause the gingival and adjacent mucosal contour to be altered when inflammation is eliminated. The shrinkage causes spaces under bridge pontics and removable bases, resulting in the accumulation of food debris and bacterial plaque, generating again the appearance of inflammation.
- Inflammation prevents locating the gingival margin of the restorations due to their permanent instability, a situation that improves when starting from a healthy or normalized gingiva.

Any restorative dentistry practice should end with the gingiva in a healthy state. Note the gingival margin, its beveled, pale pink finish, and the characteristic stippling of the inserted gingiva. A. Image of normal gingiva on two porcelain crowns, one week after final cementation. B. Twenty years later, the gingival health indicates that the restorations were made with periodontal criteria. There is no inflammation or retraction of the gingival margin.
Thank you for Reading




Responses