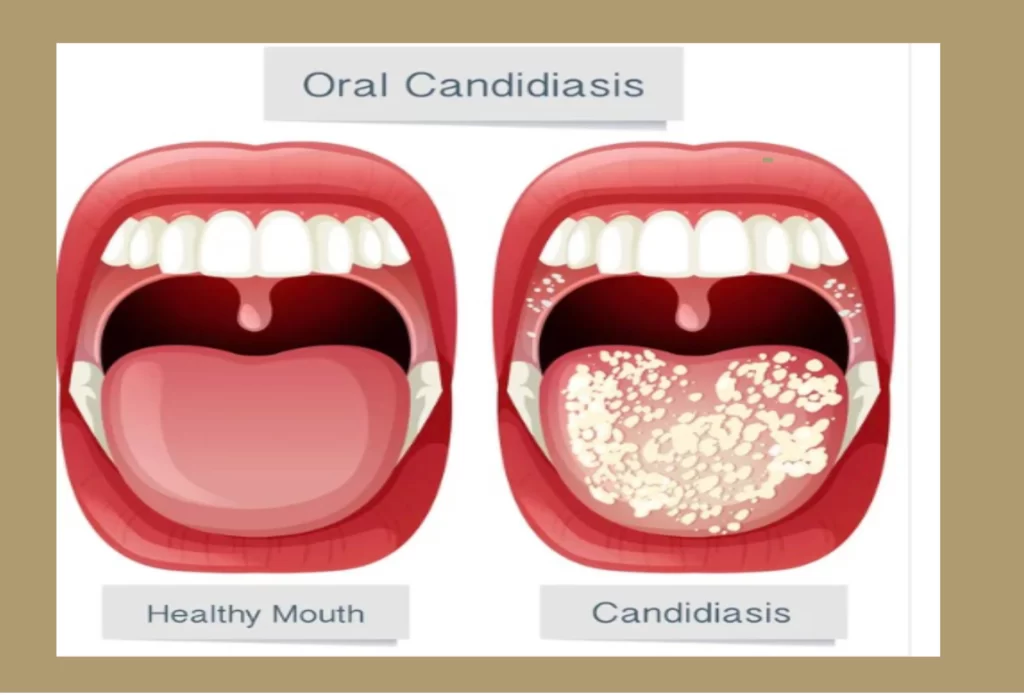
Oral Candidiasis: A Fungal Infection That Demands Attention
Introduction
Candida albicans, a species of fungi, resides harmlessly as a lifelong commensal in the human body. Although fungi make up only 7% of the approximately 8.7 million eukaryotic organisms on Earth, around 600 species are pathogenic to humans. Among these pathogenic fungi, Candida albicans, along with Cryptococcus neoformans, Aspergillus fumigatus, and Histoplasma capsulatum, poses a significant threat, causing life-threatening infections. Candida albicans is particularly responsible for a majority of hospital-related infections, presenting itself in two distinct forms: superficial candidiasis and systemic candidiasis.
Risk Factors and Predisposition
The development of oral candidiasis is strongly associated with various risk factors, with HIV infection being a major contributor. Additional factors include wearing dentures and extremes of age. Predisposing factors for candidiasis in general, though not as clearly defined as those for oral candidiasis, encompass the use of antibiotics, oral contraceptives, diabetes mellitus, pregnancy, and hormone therapy. While superficial candidiasis, although prevalent and burdensome, is non-lethal, systemic candidiasis poses a significantly higher crude mortality rate, even when treated with primary antifungal therapies.
Other potential risk factors such as venous catheters, trauma, and gastrointestinal surgeries that breach the mucosal barrier may also play a role in the development of candidiasis.
Understanding the Pathogenesis
Various factors known as virulence factors contribute to the pathogenicity of Candida albicans. These factors include morphological transitions from yeast to hyphal forms, adhesins and invasins on the cell surface, thigmotropism, secretion of hydrolytic enzymes, and the formation of biofilms.
The interaction between the candida organism and the host’s defense mechanisms plays a vital role in candida infections, as is the case with any infection affecting the human body. Lymphocytes and other nonspecific inhibitors contribute to the defense against the organism. To reach the internal surfaces of the body, the organism undergoes multiple steps, such as induced endocytosis and active penetration. Host ligands, such as E-cadherin on epithelial cells and N-cadherin on endothelial cells, act as receptors for specialized proteins on the organism’s cell surface, referred to as “invasins.”
Numerous factors and activities have been identified that contribute to the pathogenic potential of Candida albicans. These include molecules that facilitate adhesion and invasion into host cells, secretion of hydrolases, the transition from yeast to hyphal form, contact sensing and thigmotropism, biofilm formation, phenotypic switching, and various fitness attributes.
The candida organism possesses three surface adhesion molecules and an aspartyl proteinase enzyme that enables initial penetration into keratinized surfaces. Fungal adhesion and physical forces are essential for penetration. Deeper penetration is facilitated by hyphae, guided by a mechanism called “thigmotropism.” The organism switches to its hyphal form upon contact sensing, a process potentially enabled by the aspartic protease (Saps), which contributes to active penetration. On the other hand, lipases and phospholipases have not been found to significantly contribute to this process.
Two invasins have been identified: Als3 (agglutinin-like sequence), an adhesin, and Ssa1. These invasins bind to host receptors via a clathrin-dependent mechanism, resulting in endocytosis. Macropinocytosis has also been observed as another mechanism facilitating endocytosis.
The Als family gene, consisting of 8 members (Als1-7 to Als9), encodes glycosylphosphatidylinositol (GPI)-linked cell surface glycoproteins. Among them, Als3 plays a crucial role in adhesion and is upregulated during candidial infections, whether mucosal or vaginal.
Ssa1 is a cell-surface expressed member of the heat shock protein 70 (Hsp70) family.
Another significant adhesin of Candida albicans is Hwp1, a hypha-associated GPI-linked protein that forms covalent bonds with C. albicans.
Upon entering phagocytic cells, such as neutrophils or macrophages, the fungus conveniently switches between different forms. For example, in polymorphonuclear leukocytes (PML), reactive oxygen species and antimicrobial peptides are produced. The organism faces nutritional deprivation and adapts by transitioning into its hyphal form, which thrives in unfavorable environments. In macrophages, the organism switches from glycolysis to gluconeogenesis and subsequently utilizes lipids and amino acids as alternative food sources.
Pathogenicity of C. albicans:
A Complex Interplay The schematic diagram below illustrates the contribution of various virulence factors to C. albicans’ pathogenicity. Commonly, C. albicans colonizes epithelial surfaces (stage 1) and causes superficial infections (stage 2). However, when the host’s condition is compromised, the fungus penetrates deeper into the epithelial tissue, establishing deep-seated infections (stage 3). In some cases, C. albicans can cause disseminated infections (stage 4), spreading to other host tissues and potentially becoming fatal. This infectious process involves numerous virulence attributes, including adhesins, hydrolytic enzyme production (Sap proteins, phospholipases, and lipases), hypha formation, and phenotypic switching. Sap2, among other Sap proteins, is known to degrade various human proteins, including mucin, extracellular matrix proteins, immune system molecules, endothelial cell proteins, and coagulation and clotting factors. Thus, Sap proteins likely play a crucial role in all four stages of infection, greatly enhancing the pathogenic ability of C. albicans.
By utilizing creative and expressive writing techniques, incorporating a variety of figures of speech, and adding emotive language, we can convey the complex nature of Candida albicans’ pathogenicity in a more engaging and accessible manner. Varying sentence lengths and structures will help create an interesting flow and pace, while adhering to a fourth-grade reading level.
Seeking Professional Guidance
Before embarking on any treatment plan, it is essential to consult a healthcare professional for a proper diagnosis. A healthcare provider will examine the affected areas and may perform tests to confirm the presence of Candida. With their expertise, they can recommend the most suitable treatment approach based on the severity and underlying causes of the infection.
Antifungal Medications: The Frontline Defense
Antifungal medications play a vital role in the treatment of oral candidiasis. They are available in various forms, including lozenges, mouth rinses, and oral tablets. These medications work by eliminating the excessive growth of Candida, providing relief and promoting healing. It is crucial to follow the prescribed dosage and complete the full course of treatment to ensure effective eradication of the infection.
Maintaining Oral Hygiene: A Preventive Measure
Good oral hygiene practices are key to both preventing and managing oral candidiasis. Regular brushing of teeth, tongue, and gums with a soft-bristled toothbrush helps remove plaque and minimize the growth of Candida. Additionally, using an antifungal mouthwash as recommended by your dentist or healthcare provider can help keep the fungal infection at bay.
Natural Remedies: Complementary Approaches
In conjunction with conventional treatments, natural remedies can provide supportive relief from oral candidiasis. For instance, rinsing the mouth with a warm saltwater solution can help soothe discomfort and reduce inflammation. Furthermore, incorporating probiotics into your diet or taking probiotic supplements may help restore the balance of beneficial bacteria in your mouth, preventing the overgrowth of Candida.
Lifestyle Modifications: Enhancing Immunity
Boosting your immune system is crucial in combating oral candidiasis. Adopting a healthy lifestyle can significantly contribute to strengthening your immune response. Ensure a balanced diet rich in essential nutrients, vitamins, and minerals. Regular exercise, adequate sleep, and stress management techniques are equally important in fortifying your immune system and reducing the risk of fungal infections.
Conclusion
Oral candidiasis, though uncomfortable, can be effectively treated and managed with the right approach. Seeking professional guidance, utilizing antifungal medications, practicing good oral hygiene, exploring natural remedies, and adopting a healthy lifestyle are all essential strategies for combating oral candidiasis. Remember to consult with your healthcare provider for a comprehensive evaluation and personalized treatment plan. By taking proactive measures, you can achieve relief, prevent recurrences, and maintain optimal oral health. Say goodbye to oral candidiasis and embrace a life of oral wellness!





Responses