BURN

From campfires to candlelit dinners, fire has long been an integral part of human civilization. However, amidst its warmth and light, there’s a darker side to fire’s embrace—the burn. Burns, whether minor or severe, can have significant physical and psychological implications, often leaving lasting scars both on the body and the mind. In this article, we’ll delve into the multifaceted nature of burns, exploring their causes, classifications, treatments, and the emotional toll they can exact.
Understanding Burns:
Burns occur when skin comes into contact with extreme heat, electricity, chemicals, or radiation. They are classified based on their severity and depth:
1. First-Degree Burns: These affect only the outer layer of the skin, causing redness, pain, and minor swelling. Sunburns are a common example.
2. Second-Degree Burns: These penetrate the second layer of the skin, causing blisters, severe pain, and possible scarring.
3. Third-Degree Burns: The most severe type, these burns extend into deeper tissues, potentially damaging nerves, muscles, and bones. They may appear white, charred, or leathery and often require surgical intervention.
Causes of Burns:
Burns can result from various sources:
1. Heat: Contact with flames, hot objects, steam, or hot liquids can cause thermal burns.
2. Electricity: Exposure to electrical currents can lead to electrical burns, which can cause internal damage even if the skin appears unaffected.
3. Chemicals: Contact with corrosive substances like acids or alkalis can cause chemical burns, which can continue to damage tissue until the chemical is neutralized or removed.
4. Radiation: Overexposure to ultraviolet (UV) radiation from the sun or artificial sources like tanning beds can lead to radiation burns, commonly known as sunburns.
The mechanism of injury in burns involves a complex interplay of various factors depending on the type and source of the burn. Here’s an overview of the mechanisms involved in different types of burns:
1. Thermal Burns:
– Direct Contact: The most common cause of thermal burns is direct contact with a heat source such as flames, hot liquids, steam, or hot surfaces. The heat energy transfers to the skin, causing tissue damage.
– Radiant Heat: Burns can also occur due to exposure to radiant heat from sources like fires or explosions, even without direct contact. The heat radiates from the source and heats the skin, causing burns.
– Flash Burns: These occur due to brief exposure to intense heat, often associated with explosions or flash fires. The rapid heat transfer can cause significant burns to exposed skin.
2. Electrical Burns:
– Electric Current: Electrical burns result from contact with electrical currents. The current passes through the body, generating heat as it encounters resistance in tissues. The heat causes thermal injury to the skin and underlying tissues along the path of the current.
– Entrance and Exit Wounds: Electrical burns often have entry and exit points where the current enters and exits the body, causing localized burns at these sites. The severity of the burns depends on factors such as voltage, current intensity, duration of contact, and the pathway the current takes through the body.
3. Chemical Burns:
– Corrosive Substances: Chemical burns occur when the skin comes into contact with corrosive or caustic substances such as acids, alkalis, solvents, or industrial chemicals. These
substances cause direct damage to the skin and underlying tissues by disrupting cellular structures and functions.
– Penetration and Spread: Chemical burns can penetrate the skin layers rapidly, depending on the nature and concentration of the chemical involved. Some chemicals may continue to cause damage even after the initial contact, as they penetrate deeper into the tissues or spread across the skin surface.
4. Radiation Burns:
– Ultraviolet Radiation: Radiation burns, commonly known as sunburns, result from overexposure to ultraviolet (UV) radiation from the sun or artificial sources such as tanning beds. UV radiation damages the DNA in skin cells, leading to inflammation, redness, blistering, and pain.
– Ionizing Radiation: Exposure to ionizing radiation, such as X-rays or radioactive materials, can cause radiation burns by damaging cells and tissues at the molecular level. The severity of radiation burns depends on factors such as the dose, duration of exposure, and the sensitivity of the exposed tissues.
Understanding the specific mechanisms of injury in burns is crucial for effective prevention, management, and treatment. Prevention strategies often focus on safety measures to avoid exposure to heat sources, electrical hazards, corrosive chemicals, and excessive sun exposure. Additionally, prompt and appropriate first aid and medical care are essential to minimize the extent of tissue damage and improve outcomes for burn victims.
The Psychological Impact:
Beyond the physical pain and discomfort, burns can have profound psychological effects:
1. Emotional Trauma: Survivors of severe burns often experience trauma related to the event itself, as well as the ongoing challenges of recovery and rehabilitation.
2. Body Image Issues: Visible scarring from burns can lead to self-consciousness and diminished self-esteem. Coping with altered physical appearance may require extensive psychological support.
3. Post-Traumatic Stress Disorder (PTSD): Some individuals may develop PTSD following a burn injury, experiencing flashbacks, nightmares, and anxiety related to the traumatic event.
Classification of Burns: Degrees, size and TBSA
Degrees of Burns:
Burns are typically classified into three main degrees based on their severity:
1. First-Degree Burns:
– Superficial burns that only affect the outer layer of the skin, known as the epidermis.
– Symptoms include redness, pain, and mild swelling.
– Common causes include sunburn, brief contact with hot objects or liquids.
– First-degree burns usually heal within a few days with basic first aid like cool water, moisturizing, and over-the-counter pain relievers.
2. Second-Degree Burns:
– Affect both the epidermis and the underlying layer, the dermis.
– Symptoms include blistering, severe pain, swelling, and redness.
– Common causes include scalding liquids, contact with hot objects, or prolonged exposure to the sun.
– Treatment often involves keeping the area clean, applying antibiotic ointment, and sometimes covering with a sterile dressing. Severe cases may require medical attention to prevent infection and promote healing.
3. Third-Degree Burns:
– The most severe type of burn, affecting all layers of the skin and potentially underlying tissues, nerves, and muscles.
– Symptoms may include charred or white skin, numbness due to nerve damage, and a leathery texture.
– Causes include prolonged exposure to flames, chemicals, or extremely hot objects.
– Treatment requires immediate medical attention. It may involve surgery, skin grafts, and intensive wound care to prevent complications such as infection and scarring.
Classification by Size:
Burn size is typically measured as a percentage of the total body surface area (TBSA) affected. This measurement helps healthcare professionals assess the severity of the burn and determine the best course of treatment. Burns are often categorized into the following classifications based on size:
1. Minor Burns:
– Usually involve less than 10% of TBSA in adults or less than 5% in children.
– These burns are typically considered minor and can often be managed with basic first aid at home, such as cool water irrigation, cleaning, and applying a sterile dressing.
2. Moderate Burns:
– Involve between 10% to 20% of TBSA in adults or between 5% to 10% in children.
– Moderate burns may require medical attention, including pain management, wound cleaning, and possibly topical treatments like antibiotic ointments or dressings.
3. Severe Burns:
– Include burns affecting more than 20% of TBSA in adults or more than 10% in children.
– Severe burns are considered medical emergencies and require immediate professional intervention. Treatment may involve fluid resuscitation, wound debridement, intravenous antibiotics, and possibly surgical interventions like skin grafting.
Implications of Burn Size:
The size of a burn can have significant implications for the patient’s prognosis and recovery process. Larger burns are associated with:
- Fluid Loss and Shock: Extensive burns can lead to significant fluid loss through damaged skin, potentially resulting in hypovolemic shock, a life-threatening condition.
2. Infection Risk: Large burns create a favorable environment for bacterial growth and increase the risk of infection, which can further complicate treatment and delay healing.
3. Systemic Effects: Severe burns can trigger systemic inflammatory responses, leading to complications such as organ dysfunction, respiratory distress, and metabolic imbalances.
Calculating the total body surface area (TBSA) affected by a burn is essential for determining the severity of the injury and guiding treatment decisions. There are several methods for estimating TBSA, with the Rule of Nines and the Lund and Browder Chart being the most commonly used in clinical practice. Here’s how you can calculate TBSA using both methods:
1. Rule of Nines:
The Rule of Nines is a quick and easy method for estimating TBSA in adults. It divides the body into regions, each representing approximately 9% or a multiple of 9% of the total body surface area. The regions include:
– Head and neck: 9%
– Each arm: 9% (total for both arms is 18%)
– Each leg: 18% (total for both legs is 36%)
– Anterior trunk: 18%
– Posterior trunk: 18%
– Genital area: 1%
To calculate TBSA using the Rule of Nines:
– Assess the percentage of each region affected by the burn.
– Sum the percentages of all affected regions to determine the total TBSA.
2. Lund and Browder Chart:
The Lund and Browder Chart provides a more precise estimation of TBSA, especially for burns involving children or burns with irregular shapes. This method divides the body into smaller segments, with varying percentages of TBSA for each segment depending on the age of the individual. The chart provides specific percentages for each body part at different age ranges.
To calculate TBSA using the Lund and Browder Chart:
– Assess the percentage of each body segment affected by the burn.
– Multiply the percentage of each segment by its corresponding TBSA value from the chart.
– Sum the products of all affected segments to determine the total TBSA.
It’s important to note that these methods provide estimates, and the actual TBSA may vary based on factors such as body habitus, age, and the presence of pre-existing medical conditions. Additionally, for burns involving children, healthcare providers may use age-adjusted formulas or charts to account for differences in body proportions and surface area distribution.
Accurate calculation of TBSA is crucial for determining the severity of burns, guiding fluid resuscitation, and assessing the need for specialized care in burn centers. In cases of extensive burns or uncertainty in estimation, consulting with a burn specialist is recommended for appropriate management.
TBSA in children:
Calculating the Total Body Surface Area (TBSA) involved in burns in children requires special consideration due to differences in body proportions compared to adults. Several methods and charts have been developed specifically for estimating TBSA in pediatric patients. The most commonly used method is the Lund and Browder Chart, which provides age-specific estimates of TBSA for different body regions.
The Lund and Browder Chart divides the body into anatomical regions, each assigned a percentage of TBSA based on the age of the child. The percentages for each body region may vary depending on the child’s age due to differences in body proportions and growth. Here’s a general overview of the Lund and Browder Chart for estimating TBSA in children:
1. Head and Neck:
– This region typically represents about 18% of TBSA in infants and young children.
2. Upper Limbs (Arms):
– Each arm is usually assigned a TBSA percentage ranging from 9% to 12%, depending on the child’s age.
3. Trunk:
– The anterior trunk (front of the body) and the posterior trunk (back of the body) together account for a varying percentage of TBSA, typically ranging from 18% to 27% depending on the child’s age.
4. Lower Limbs (Legs):
– Each leg is generally assigned a TBSA percentage ranging from 13% to 18%, depending on the child’s age.
5. Genitalia:
– The genitalia region typically represents about 1% of TBSA in both males and females.
NOTE: When estimating TBSA in children using the Lund and Browder Chart:
– Assess the extent of burn injury in each anatomical region.
– Multiply the percentage of TBSA assigned to each region by the child’s age-specific value.
– Sum the products for all affected regions to determine the total TBSA.
-It’s important to note that the Lund and Browder Chart provides estimates and may not account for individual variations in body size and shape. Additionally, the chart does not consider the percentage of TBSA involved in burns affecting smaller areas or irregularly shaped burns. In such cases, healthcare providers may use other methods, such as the Rule of Nines or specialized pediatric burn assessment tools, to estimate TBSA accurately.
Systemic response to burn:
Burn injuries trigger a complex systemic response that affects various physiological systems in the body. Understanding these systemic responses is essential for managing burn patients effectively. Here’s how burns impact different body systems:
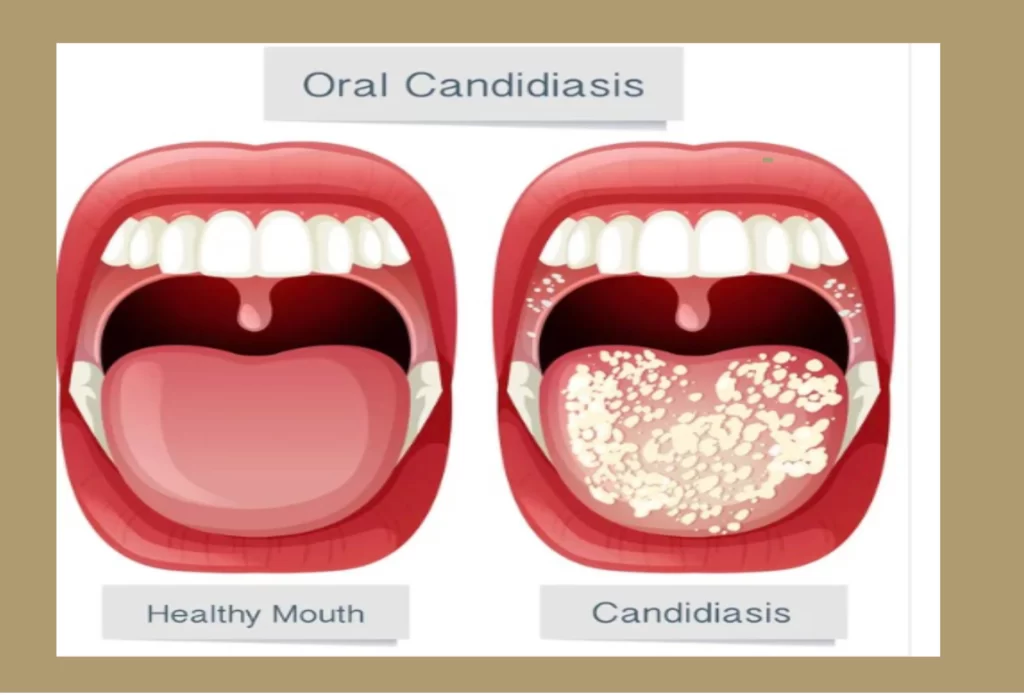
1. Integumentary System (Skin):
– The skin is the primary barrier against infection and regulates body temperature.
– Burn injuries compromise the skin’s integrity, leading to increased susceptibility to infection, fluid loss, and temperature dis-regulation.
– Severe burns can result in extensive tissue damage, requiring surgical interventions like skin grafting to promote wound healing and prevent complications.
2. Cardiovascular System:
– Burn injuries can cause a systemic inflammatory response, leading to fluid shifts and increased capillary permeability.
– Initially, there is a hypovolemic state due to fluid loss into the burn wound and surrounding tissues, resulting in decreased cardiac output and hypotension.
– Over time, the body may enter a hyper-dynamic state characterized by increased heart rate, cardiac output, and peripheral vascular resistance in response to the inflammatory cascade.
3. Respiratory System:
– Inhalation injuries, common in burns involving fires or hot gases, can lead to airway compromise and respiratory distress.
– Direct thermal injury to the airway can cause edema, inflammation, and obstruction, requiring immediate airway management and possibly intubation.
– Systemic inflammation and fluid shifts can also contribute to pulmonary edema and acute respiratory distress syndrome (ARDS), further compromising respiratory function.
4. Renal System:
– Burn injuries can lead to acute kidney injury (AKI) due to hypovolemia, decreased renal perfusion, and systemic inflammatory response.
– The kidneys play a crucial role in fluid balance and electrolyte regulation, and AKI can result in electrolyte imbalances, metabolic acidosis, and fluid overload.
5. Gastrointestinal System:
– Burn injuries can lead to decreased gastrointestinal perfusion and mucosal damage, resulting in decreased gut motility and increased risk of bacterial translocation.
– Patients may develop stress ulcers, ileus and malabsorption, necessitating early enteral nutrition and gastric protection with proton pump inhibitors.
– Systemic inflammatory response can also contribute to increased intestinal permeability, leading to endotoxemia and systemic complications.
6. Immune System:
– Burn injuries suppress the immune system, making patients more susceptible to infections, particularly from opportunistic pathogens.
– The systemic inflammatory response can lead to a cytokine storm, contributing to multi-organ dysfunction syndrome (MODS) and sepsis.
– Burn patients may require prophylactic antibiotics, meticulous wound care, and immunomodulatory therapy to prevent and manage infections.
7. Metabolic System:
– Burn injuries increase metabolic demands due to the hyper-metabolic response characterized by elevated catecholamine levels, increased oxygen consumption, and protein catabolism.
– Patients may experience hyperglycemia, insulin resistance, and muscle wasting, necessitating aggressive nutritional support and metabolic monitoring.
– Burn-induced hyper-metabolism can persist for weeks to months, requiring long-term nutritional interventions to support wound healing and mitigate complications.
Admission criteria for burn wound:
Admission criteria for burn wound management vary depending on the severity of the burn injury, the resources available at the healthcare facility, and the expertise of the healthcare providers. However, certain criteria are commonly used to determine the need for admission to a burn unit or hospitalization for burn wound management.
These criteria typically include:
1. Extent of Burn Injury:
– Burns involving a significant percentage of the total body surface area (TBSA), especially those exceeding 10% TBSA in adults or 5% TBSA in children, often require hospital admission.
-The presence of burns affecting critical areas such as the face, hands, feet, genitalia, or major joints may also warrant admission for specialized care.
2. Depth and Severity of Burns:
– Deep partial-thickness (second-degree) burns and full-thickness (third-degree) burns generally necessitate hospital admission for proper assessment, wound care, and potential surgical intervention.
– Burns associated with complications such as inhalation injury, electrical injury, or circumferential burns requiring escharotomies may require admission to a burn center or specialized facility.
3. Presence of Inhalation Injury:
– Inhalation injuries, characterized by exposure to smoke, toxic gases, or hot air, can cause airway compromise, respiratory distress, and pulmonary complications.
– Patients with suspected or confirmed inhalation injury often require close monitoring and may need admission to an intensive care unit (ICU) or burn center for airway management and respiratory support.
4. Associated Injuries or Comorbidities:
– Burn patients with concomitant injuries such as fractures, head trauma, or other trauma requiring surgical intervention may require admission for comprehensive management.
– Patients with pre-existing medical conditions, such as cardiovascular disease, diabetes, or immunosuppression, may be at higher risk of complications and may benefit from hospitalization for close monitoring and specialized care.
5. Age and Vulnerability:
– Pediatric patients, elderly individuals, and patients with impaired mobility or cognitive function may have unique care needs and may require admission for close observation and specialized care.
6. Resource Availability:
– Availability of resources, including burn units, specialized equipment, and trained personnel, may influence the decision to admit patients for burn wound management.
– Patients requiring complex interventions such as surgical debridement, skin grafting, or burn rehabilitation may need access to specialized facilities and expertise available in tertiary care centers or burn centers.
7. Social and Environmental Factors:
– Consideration of social factors such as access to follow-up care, availability of caregiver support, and living conditions that may impact wound healing and rehabilitation is important in determining the need for admission.
It’s essential for healthcare providers to assess each burn patient individually, taking into account the specific characteristics of the burn injury, associated injuries or comorbidities, and available resources to make informed decisions regarding admission for burn wound management. Collaboration among burn care specialists, emergency physicians, surgeons, and other healthcare professionals is crucial in providing optimal care for burn patients.
Management:
The management of burns, particularly larger ones, requires a multidisciplinary approach involving specialized burn care teams. Treatment strategies may include:
- Fluid Resuscitation: Administering intravenous fluids to maintain adequate hydration and prevent shock.
2. Wound Care: Cleaning and debriding the burn wounds to remove dead tissue and reduce the risk of infection.
3. Pain Management: Providing analgesics to alleviate pain associated with the burn injury and subsequent treatments.
4. Surgical Interventions: Performing surgical procedures such as skin grafting to promote wound healing and minimize scarring.
The management of burns depends on their severity:
1. First-Degree Burns: These can often be treated with simple first aid measures such as running cool water over the affected area, applying soothing lotions like aloe vera, and taking over-the-counter pain relievers.
2. Second-Degree Burns: More extensive burns may require professional medical attention. Cleaning the wound, applying antibiotic ointments, and covering it with sterile dressings are common practices. In severe cases, skin grafts may be necessary to promote healing and reduce scarring.
3. Third-Degree Burns: These typically require immediate medical attention. Treatment may involve debriding the wound (removing dead tissue), administering intravenous fluids to prevent dehydration, and providing pain management. In many cases, specialized burn centers with multidisciplinary teams are essential for optimal care.
The primary objective of burn management:
-is to provide comprehensive care to individuals with burn injuries, addressing both the immediate and long-term consequences of the injury. The overarching goals of burn management include:
1. Immediate Stabilization and Assessment:
– Prioritize the ABCs (Airway, Breathing, Circulation) and ensure that the patient’s vital functions are stable.
2. Prevention of Further Injury:
– Remove the patient from the source of the burn and prevent additional exposure to heat, chemicals, or other harmful agents.
– Secure the airway and provide respiratory support if necessary, especially in cases of inhalation injury or airway compromise.
3. Pain Management and Comfort:
– Administer analgesics to alleviate pain associated with the burn injury, wound care procedures, and subsequent treatments.
– Consider both pharmacological and non-pharmacological interventions to optimize pain control and promote patient comfort.
4. Wound Care and Dressing:
– Initiate prompt wound care measures to prevent infection, promote wound healing, and minimize scarring.
– Cleanse the burn wounds thoroughly, remove necrotic tissue, and apply appropriate dressings to create a moist wound environment conducive to healing.
5. Fluid Resuscitation and Hemodynamic Support:
– Calculate fluid requirements based on the extent of burn injury and the patient’s clinical status, aiming to restore and maintain adequate tissue perfusion.
– Monitor fluid balance closely, titrate fluid administration based on clinical response, and adjust management accordingly to prevent hypovolemic shock or fluid overload.
6. Prevention and Management of Complications:
– Anticipate and address potential complications associated with burn injuries, including infection, respiratory compromise, acute kidney injury, and systemic inflammatory response syndrome (SIRS).
– Implement preventive measures such as early enteral nutrition, pressure ulcer prevention, and deep vein thrombosis prophylaxis to reduce the risk of complications.
7. Psychosocial Support and Rehabilitation:
– Provide emotional support, counseling, and resources to help patients cope with the physical and psychological impacts of burn injuries.
– Facilitate multidisciplinary rehabilitation services, including physical therapy, occupational therapy, and psychosocial support, to optimize functional outcomes and quality of life.
8. Long-Term Follow-Up and Scar Management:
– Establish a comprehensive follow-up plan to monitor wound healing, assess functional recovery, and address long-term sequelae such as hypertrophic scarring and contractures.
– Implement scar management strategies, including pressure garments, silicone gel sheets, and scar massage, to minimize scar formation and improve cosmetic and functional outcomes.
What to do at home before, medical intervention:
Before seeking medical attention for a burn injury, there are several essential steps you can take at home to provide immediate first aid and minimize further damage. Here’s what to do for minor to moderate burns before going to the hospital:
1. Remove the Source of Heat:
– If the burn was caused by a hot object, liquid, or flame, move away from the heat source immediately to prevent further injury.
2. Cool the Burn:
– Hold the burned area under cool (not cold) running water for 10-20 minutes to reduce pain, swelling, and further tissue damage. Avoid using ice or ice-cold water, as it can cause frostbite and exacerbate the injury.
3. Remove Constrictive Items:
– If the burn occurred on an area with jewelry, clothing, or accessories, carefully remove any constrictive items to prevent constriction or swelling.
-In the case of chemical burns, it’s crucial to flush the affected area with water continuously until medical help arrives.
4. Protect the Burned Area:
– Cover the burn with a clean, dry cloth or sterile dressing to protect it from contamination and reduce the risk of infection. Avoid applying creams, ointments, or home remedies to the burn as they may trap heat and worsen the injury.
5. Manage Pain:
– Over-the-counter pain relievers such as ibuprofen (Advil) or acetaminophen (Tylenol) can help alleviate pain associated with the burn injury. Follow the recommended dosage instructions.
6. Seek Medical Advice:
– Determine whether medical attention is necessary based on the severity of the burn. Minor burns may be manageable at home with first aid, while moderate to severe burns require medical evaluation and treatment.
7. Stay Hydrated:
– Drink plenty of fluids to stay hydrated, especially if the burn covers a large area of the body. Dehydration can exacerbate the effects of the burn injury.
NOTE: It’s important to note that these steps are for immediate first aid and should not replace professional medical evaluation and treatment.
Prevention:
Preventing burns involves taking appropriate safety measures, including:
1. Using caution around hot objects and liquids.
2. Installing smoke detectors and fire extinguishers in homes and workplaces.
3. Handling chemicals with care and wearing appropriate protective equipment.
4. Following electrical safety guidelines and avoiding overloaded circuits.
In summary, burn injuries elicit a profound systemic response involving multiple organ systems. Management of burn patients requires a multidisciplinary approach, addressing not only the local wound care but also the systemic effects to optimize outcomes and reduce morbidity and mortality. Early recognition of systemic complications and timely interventions are critical in improving patient outcomes in burn care.
Conclusion:
– Burns are not merely physical injuries; they encompass a complex interplay of physical and psychological factors. While advances in medical science have improved outcomes for burn victims, comprehensive care must address both the visible and invisible scars left by these traumatic events. By understanding the causes, classifications, treatments, and emotional implications of burns, we can better support those affected and work towards their physical and psychological healing.
– Burn management aims to optimize patient outcomes, reduce morbidity and mortality, and promote the physical and psychosocial well-being of individuals affected by burn injuries. A multidisciplinary approach involving burn care specialists, nurses, therapists, and support staff is essential in achieving these goals and providing comprehensive care throughout the continuum of burn injury management.




Responses